6 min read
It’s time for doctors to join a public debate on Covid policies and treatments
By: AMPS - Australian Medical Association on May 23, 2023 6:25:49 PM
‘If the freedom of speech is taken away, then dumb and silent we may be led, like sheep to the slaughter.’ – George Washington.
Two days prior to his death, an apparently healthy George Washington had ridden around his estate on a cold wet day. Not wanting to keep guests waiting for dinner, he did not change out of his wet clothes. He felt sick a day later, developing a throat infection. He was given a mixture of butter, molasses, and vinegar to no avail. His team of doctors administered the medical therapy that had been used for at least 3,000 years since the time of Ancient Egypt, bloodletting. This was an attempt to balance the ‘humors’ in the body. In all, he underwent about four episodes of bloodletting, resulting in a loss of about 40 per cent of his blood volume. He died within the day after the bloodletting.
Though bloodletting was already being questioned in the 16th century, Dr Benjamin Rush, a prominent public health advocate, signer of the Declaration of Independence, Chief Physician of the Revolutionary Army, esteemed physician, and educator, was an aggressive proponent of bloodletting. According to Dr Rush, all significant illness resulted from increased vascular tension, which was best treated by applying ‘depletion theory’ which consisted of aggressive bloodletting and a mercury-based purgative. His prominent bully pulpit likely influenced greatly the practise of doctors of the day, including George Washington’s team of doctors.
In 1793, there was a yellow fever epidemic in Philadelphia that had killed nearly 10 per cent of the population. Dr Rush claimed that bloodletting for this disease would increase survival rates. He was challenged by the unlikeliest of people, ‘Peter Porcupine’ a pseudonym used by William Corbett, a British journalist writing in the Porcupine’s Gazette. Sadly at that time, the debate over the appropriate treatment of yellow fever was seemingly tied to political affiliations, with the Republicans (including Rush and Thomas Jefferson) bitterly opposed by the Federalists (including Hamilton). The debate was extremely vitriolic, with Corbett at one time saying:
‘Rush … seized with uncommon alacrity and address, the occasion presented by yellow fever, the fearful ravages of which were peculiarly calculated to dispose the minds of panic struck people to the tolerance, and even admiration, of experiments, which, at any other time, they would have rejected with disdain.’
These attacks, which further included branding Rush ‘The Bleeding Physician of Philadelphia’, had the effect of reducing the number of patients who sought his business. He sought legal remedies by bringing one of the first professional libel suits in the United States against William Corbett. The case was only heard two years later, in front of not too friendly a judge, and ultimately, William Corbett lost, and had to pay Rush $5,000, one of the largest libel awards at that time. Ironically, the verdict was rendered on December 14, 1799, the same day President Washington lay on his deathbed, being bled dry by a colleague and pupil of Rush.
Undeterred, Corbett continued his criticism of Rush after the verdict, albeit now with a new publication Rush-Light. In a February 1800 edition, using municipal records, he presented data on mortalities during the 1793 yellow fever epidemic. Comparing the average monthly deaths, he showed deaths were much higher in the months following Rush’s implementation and advertisement of his treatment, compared to the months prior.
The tide was turning elsewhere as well. In Paris, Dr Pierre Louis, a physician, assessed the efficacy of bloodletting in the treatment of pneumonia and tracked the outcomes of 77 carefully selected patients. He concluded that ‘the effect of this procedure was much less than commonly believed’. Subsequent studies by Pasteur, Koch, and Virchow further confirmed the findings justifying criticism towards bloodletting as a therapy for such conditions, and its use currently in modern medicine is limited to a few select conditions.
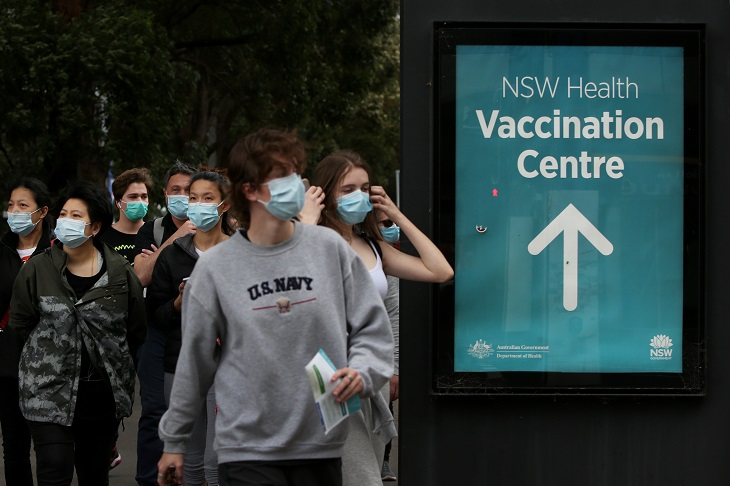
As doctors today, first of all, we are relieved at this scientific evolution harnessed as a result of vigorous debate over data. Mainly, we could not contemplate the bloodletting that might have had to take place had the practise persisted another 220 years and made its way to the top of ATAGI recommendations. We have seen censorship unparalleled in the scope of its reach in human history, especially in the treatment of Covid. Doctors who have dissented from official state-sanctioned treatment diktats have been and continue to be sanctioned by the medical regulator, and egregiously unfairly fired from their positions.
The restrictions on prescribing ivermectin have recently been dropped by the TGA. The provisionally approved Covid vaccines have been associated with unprecedented harm and demonstrated negative efficacy; alarmingly, there are still official recommendations for their continued usage.
The unprecedented squashing of scientific debate by the regulatory authorities enabled by MainStream Media and social media censorship, which continues to this day, is a major block to the advancement of healthcare in this country and around the world. This is highly destructive to the foundations of an open and free democracy. If the medical profession is happy to unquestioningly accept the dictates of health bureaucrats instead of scientific debate, this is to the detriment of patients’ health.
The doctors at the Australian Medical Professionals Society have invited the doctors of the Australian Medical Association to a public debate on the government’s response to Covid with a particular focus on the safety and efficacy of the provisionally approved Covid vaccines. Health Professionals must be free to publicly debate public policy using the most up to date scientific evidence and their clinical judgment, unhindered by government regulatory censorship. We would also like to debate the ethical egresses forced on the medical profession and the public by the imposition of mandates.
In modern medicine, our symbol is that of a Physician’s staff with an Asclepiusian snake wrapped around it. Asclepius was the Greek God of healing, and Hippocrates was a student of his. Asclepius made use of a magic potion, which when drawn from the right side of the Gorgon would kill, and from the left side could cure. It speaks to the duality as our role as healers, we seek to heal, but we also have the capacity to harm. The way we minimise harm to our patients is to always allow open discourse, and courteous dialogue amongst health professionals so that the best ideas can prevail.
Dr Aseem Malhotra, a prominent British cardiologist who famously reversed his position on Covid vaccines, is touring Australia with doctors from AMPS from May 27, 2023. Whilst many of the events are open to the public, there are some events planned in Melbourne, Sydney, and Brisbane only for health professionals. In Melbourne and Sydney, whilst addressing healthcare practitioners, Dr Malhotra will be joined by Emeritus Professor Robert Clancy, a distinguished Australian Immunologist. In Brisbane, he will be joined by Professor Wendy Hoy, another distinguished Australian physician whilst addressing healthcare practitioners. We urge all interested healthcare practitioners, regardless of their union affiliations, to come to these events with an open mind. One of the Malhotra’s tour goals is to get the scientific discussion and debate happening amongst a much larger section of the health professional community. Not only to discuss what went wrong with the Covid response but how we can improve systems management and improve healthcare in the future and avoid the policy and decision making disasters that occurred in Covid from ever happening again. Our profession will benefit from this, and ultimately so will our patients.
Article co-authored by Assoc Professor Chris Neil, Dr Duncan Syme, and Dr Jeyanthi Kunadhasan.
Related Posts
Did the ivermectin ban cost lives?
Censorship: a threat to public health and safety?
Practitioners are the bulwark between people, weak or corrupt leaders, captured authorities, and...


